Didactics
In the course of five years of Otolaryngology training, the residents learn the latest methods of diagnosis and treatment of congenital, infectious, metabolic, and neoplastic diseases of the ear, nose, throat, head, and neck. By graduation, their expertise encompasses head and neck cancer; facial plastic surgery; trauma and reconstructive surgery; rhinology and sinus surgery; otology/neurotology; skull base surgery; surgery of the salivary, thyroid and parathyroid glands; laryngology; bronchoesophagology; allergy and immunology; pediatric otolaryngology; and speech and swallowing pathology.
The residents learn to use innovative therapies such as laser surgery, radiofrequency tissue ablation, computerized image-guided endoscopic sinus surgery, transnasal esophagoscopy, microvascular surgery, osseointegrated implant surgery, cochlear implants, sialoendoscopy, and microneurologic procedures of the skull base.
In addition to this foundation of medical knowledge, the residents are taught state-of-the-art techniques. They learn how to perform videostroboscopy, video-naso-endoscopy, FEES, TNE, and videofluoroscopy, and how to use these techniques in the evaluation of laryngeal and velopharyngeal disorders, as well as in oropharyngeal dysmotility. The residents also learn how to conduct audiometric, tympanometric, and auditory brainstem response tests. The residents are taught all this in weekly seminars and conferences, which occur during protected time on regular workdays. Specialists who have direct experience in their subject give didactic conferences.
Didactic laboratory courses for residents are included each year. They are a head and neck dissection course with cadavers, temporal bone dissection course, plating and local flap workshop, and endoscopic sinus surgery workshop with cadavers. PGY-1 and PGY-2 residents attend a boot camp at the beginning of each academic year.
In addition to the residents' didactic lectures, continuing medical education and patient care lectures are mandatory. A head and neck oncology patient conference occurs weekly. Seminars in the principles of basic science research occur every two weeks. Grand rounds are given each month by specialists in their field at the medical center or from outside institutions. Journal Club evaluation of articles in our literature occurs each month. Morbidity and mortality review is held monthly. Each resident gives one grand round a year which consists of an exhaustive review of a specific topic related to a patient case presentation. The residents develop a quality improvement project which they complete during training and are expected to complete one or more research projects concentrated during the research block time available during residency training.
Funds are provided for residents to attend national meetings or courses, in addition to local or regional meetings. Supplemental travel money will be provided for residents who will be presenting papers, posters, abstracts or lectures.
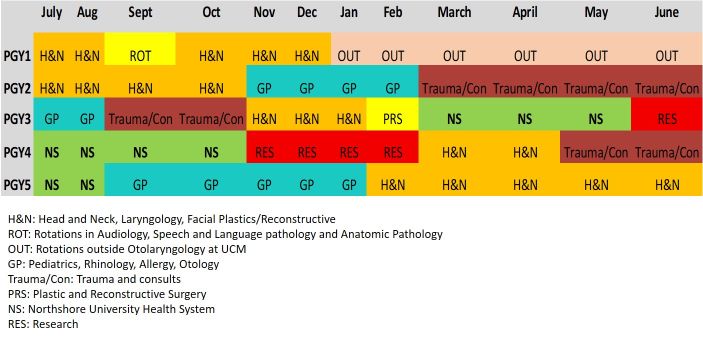
Rotation Schedule
The preliminary year of training (PGY1) will include six months of rotations in Otolaryngology. During this block, the resident will be on the Head and Neck team and the Trauma/Consult team. During this time, there will be 3 dedicated one week rotations in Audiology, Speech and Language pathology, and Anatomic Pathology. During these blocks, the resident will be supervised by faculty in the designated fields and will be given reading material to familiarize his/herself with the subject matter. In Audiology, the resident will become familiar and able to perform all audiologic and vestibular tests. In Speech and Language pathology, the resident will become familiar with swallowing evaluations such as FEES (flexible endoscopic evaluation of swallowing) and OPM (oro-pharyngeal motility), speech and swallowing support for the head and neck cancer patient, and evaluation and management of the professional voice. In Anatomic Pathology, the resident will review slides related to the head and neck and will also be supervised by faculty from the department of Pathology.
- The rest of the PGY1 year is spent rotating within the following specialties: anesthesia, general surgery, neuroradiology (a week of that rotation will be spent with radiation oncology), thoracic surgery, plastic surgery, and intensive care. Services are staffed so that the intern has maximum responsibility and opportunity for growth and development. Formal teaching programs are offered during each assignment. During the preliminary year of experience, the resident acquires expert knowledge of the pre- and post-operative care of acutely ill patients and of the principles of surgical physiology and wound management.
- Residents in the second year spend 4 months on each of the following services: Head & Neck, Trauma/Consult, and Pediatric/General Otolaryngolgy.
- Third year residents spend 9 months at the medical center, including a month-long rotation with the Plastic & Reconstructive Surgery service and a month in research. Three months of the PGY-3 year will be spent at NorthShore University Health System.
- Fourth-year residents spend 4 months at the University doing research, 4 months on clinical teams at the University, and 4 months at NorthShore.
- The fifth-year residents are at the medical center for 10 months as the chief residents with leadership and administrative responsibilities and spend two months at Northshore.
The dedicated Otolaryngology research faculty and the research interests of the clinical faculty provide excellent opportunities for resident research. The residents will take an online NIH course on proper performance of research and identify research mentors and projects during the one month research rotation during PGY3. They will carry out the identified project(s) during the 4 month block in PGY4. The interests of the basic science and clinical faculty combined encompass a wide range of research expertise in the areas of temporal bones, otology, computerized imaging, statistical analyses, allergic disease, nasal physiology, vestibular research, and oncology.
Surgical Volume
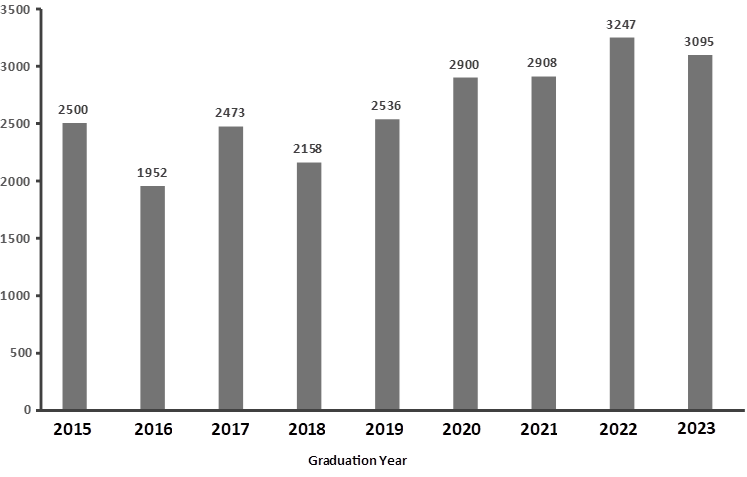
Residents typically graduate with a total of over 2000 surgical cases. These are widely distributed across subspecialties. The number of key indicator cases is on par with the national average and greatly exceeds the minimum recommended number. Figure below shows the average total number of surgical cases completed by the graduating residents over five years.